Police Recognized for Response to Persons Affected by Mental Illness
 The Hartford Police Department is pleased to announce the successful completion of the “One Mind Pledge”, a commitment the department entered to improve our response to those affected by mental health issues. The pledge is part of an initiative started by the International Association of Chiefs of Police (IACP), a professional association representing law enforcement on relevant public safety matters, including providing training and technical assistance.
The Hartford Police Department is pleased to announce the successful completion of the “One Mind Pledge”, a commitment the department entered to improve our response to those affected by mental health issues. The pledge is part of an initiative started by the International Association of Chiefs of Police (IACP), a professional association representing law enforcement on relevant public safety matters, including providing training and technical assistance.
Commitment to Partnering
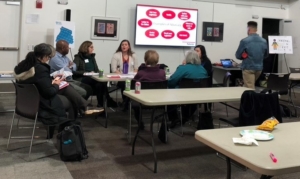
In completing the One Mind Pledge, the Hartford Police committed to a sustainable partnership with Health Care & Rehabilitative Services of Southeastern Vermont (HCRS) and other area human service providers to insure ongoing dialogue in assisting those in crisis. Through the support of HCRS, the Police Department and our community have benefited from the daily assistance of an embedded Police Social Worker, who assisted in developing model policies for the department’s response to persons in crisis.
Beyond implementing enhanced policies and meeting state legal requirements, all members of the Police Department have received enhanced Training in responding to persons experiencing a Mental Health Crisis, including one or more programs such as Mental Health First Aid, Team-Two developed by Vermont Care Partners and, CIT or Crisis Intervention Team. Assisted by HCRS, The Upper Valley Public Health Council, and the Lebanon, New Hampshire Police Department, the Police Social Worker oversees a regular CIT training program for uninformed and non-uniformed police staff, with 88% of police and communications personnel having successfully completing the program. Originally known as the “Memphis Model,” and later recommended by the President’s Task Force on 21st Century Policing, CIT is a collaborative, 40 hour program of instruction.
Preparing Law Enforcement to Respond to Persons affected by Mental Health Issues
Responding to persons affected by mental health issues, particularly those in crisis has become common for law enforcement nationwide, including the Town of Hartford. Already this year, police have answered 163 calls for persons in need of assistance due to a mental health issue. To the extreme, at least 40 were in crisis at the time officers arrived, including ten persons who were armed with weapons – including a firearm, knives and a bat. In these extreme cases, training is coupled with improved technologies and protective equipment to enhance safety for the officer and person in crisis, increasing the likelihood of a positive resolution.
The core competencies required of One Mind Pledges – collaboration, improved policies and specialized training have assisted in better preparing the Hartford Police in meeting these challenges. Although the greatest benefit is the open, continuing dialogue and collaboration with our medical, human and social service partners in preventing our residents from reaching the point of crisis.
For more information on the One Mind Pledge, including pledge requirements and a list of agencies having pledged or completed their pledge, visit the IACP website at:
https://www.theiacp.org/projects/one-mind-campaign
For more information CIT, visit the CIT International website at:
http://www.citinternational.org/What-is-CIT
— Posted with permission of Phil Kasten, Chief of Police,Town of Hartford, Vermont. Original press release dated Wednesday, December 4, 2019.