Upper Valley Community Health Equity Partnership
In March 2022, the Public Health Council signed on as the Backbone Organization for the Upper Valley Community Health Equity Partnership (UVCHEP), on behalf of the White River Junction District Office of the Vermont Department of Health. The project was funded through a US Centers for Disease Prevention and Control (CDC) grant awarded to the Vermont Department of Health (VDH) to “mobilize partners and collaborators to advance health equity and address social determinants of health as they relate to COVID-19 health disparities among populations at higher risk and that are underserved.”
The grant allowed us to bring on temporary staff to manage the project, engage local partners, and design a community-grants process. We recruited local people with personal understanding of health disparities and inequity to steer the project, providing insights, connections, and making decisions about the use of grant resources. Finally, the grant provided funds – ultimately $168,000 – for community grants that addressed a data-driven problem identified by our Steering Committee.
The UVCHEP Community Goal/Vision: The Upper Valley is a lively, growing, safe, and inclusive community where, by working together, marginalized communities have access to the power and resources necessary to ensure equitable access to health care, education, housing, food security, and other socioeconomic needs.
The UVCHeP Data Driven Problem Statement: Black, Indigenous, and People of Color (BIPOC) as well as Lesbian, Gay, Bisexual, Transgender, Queer, Intersex, Asexual and plus (LGBTQIA+) community members have higher levels of mental health challenges and substance use disorder, diagnosed and undiagnosed. These conditions are both caused by and contribute to isolation, other chronic health conditions, and not feeling safe.
 Between October 2022 and January 2023, the Steering Committee invited two rounds of grant applications, with the goal of reducing the barriers that traditionally prevent groups and organizations most closely connected to the people who experience health disparities from getting funding and other resources to address health disparities in their own communities. The Steering Committee selected ten (10) organizations to receive grants ranging roughly from $6,000 to $35,000. The grant period ran from December 2022 through November 2023, with some variation in project dates.
Between October 2022 and January 2023, the Steering Committee invited two rounds of grant applications, with the goal of reducing the barriers that traditionally prevent groups and organizations most closely connected to the people who experience health disparities from getting funding and other resources to address health disparities in their own communities. The Steering Committee selected ten (10) organizations to receive grants ranging roughly from $6,000 to $35,000. The grant period ran from December 2022 through November 2023, with some variation in project dates.
We are pleased to share the community projects with our community. Below are summaries of each of the organizations and projects. We have provided links to other sources of information when available. In a few cases, we have provided links to additional posts that the projects created to tell their own story.
Abenaki Garden
The Abenaki Garden project is providing food, teaching Abenaki gardening, culture and history in the Upper Valley. Planning began 2 years ago, and work started at the garden in August 2022 to prepare the space for winter and plant some trees and bushes. The “Abenaki Garden” project presents traditional Abenaki agriculture to the public. Utilizing food source trees, berries, herbs and vegetable varieties native and cultivated for thousands of years in Vermont, the garden recreates the concept of N’dakinna (New England) before 1492. A Fire Circle also creates a place for Abenaki speakers to tell stories, teach Abenaki culture and perform public ceremonies for public education events. Inspiration to create this space came upon reading a plea from an Abenaki Chief asking folks with land and gardens to take their gifts of ancient seeds and grow them to share the food with the tribe because they had lost all their land and needed the food. Thus, the true purpose of this project is to grow food for the Abenaki Peoples. Seeds for the project are donated by Abenaki Bands. Funds helped buy materials to construct the fencing, build a rain barrel watering system, compost, trees, bushes, and supplies. More about the Abenaki Garden.
AthletaFit
AthletaFit provides an online 8-week strength training program through the Trainerize app, with the support of a trainer with experience of the BIPOC and LGBTQIA+ community. Grant funding allowed the grantee to develop marketing and outreach to members of the BIPOC and LGBTQIA+ communities in the Upper Valley. AthletaFit seeks to address the health disparities of higher levels of mental health challenges and substance use disorder by reducing isolation and improving chronic health conditions among these underserved populations. Look for VT AthletaFit on Facebook at: https://www.facebook.com/VTAthletaFit
Community Resilience Organizations
Community Resilience Organizations of Vermont (CROs) support grassroots community organizing by people most likely to be harmed by and marginalized by large scale emergencies, such as Hurricane Irene and the COVID pandemic. CROs’ programs support the health and wellbeing of grassroots organizers in underserved, marginalized communities, and scales them up with a concerted geographical focus. As part of this grant, CROs built out their Community Wellness Program and Grassroots Organizing Hub in the White River Junction area with programs designed for BIPOC, LGBTQA, and other marginalized grassroots organizers. The goal is twofold: 1) to offer “community wellness gifts” to marginalized and unpaid organizers who experience burn-out or trauma as a result of their work and 2) to engage with new healing practitioners in providing these gift services as paid for by CROs. More about CROs.
Liberation Library (Every Town)
The Liberation Library is a space for BIPOC in the Upper Valley to gather, create, learn, and share. The library offers books, tools, art supplies and digital resources on loan at no cost and also serves as a gathering place for events, performances, craft shows and more and will be a model shared with other communities. The Liberation Library strengthens several current partnerships with New England Farmers of Color’s (NEFOC) Every Town project. For example, Vermont Releaf Collective members have access to all programming. With over 260 Releaf members, a large concentration of whom are in the Upper Valley, this serves as a central gathering and sharing place for members of this virtual BIPOC Vermonters collective. The Neighbors Network holds anti-oppression book groups and skill shares, increasing the number and quality of anti-oppression trainings and skill shares available in the area as well as increasing conversation about race and the associated awareness and solidarity in our communities and Just Construction, a collective of volunteer carpenters, offers free building and tool safety classes. You can learn more about the Liberation Library at Vermont Public and about the NEFOC at: https://nefoclandtrust.org/.
One Heart Wellness Cooperative
One Heart Wellness Cooperative is a cooperative local space where member organizations and individuals can enjoy and offer quality, accessible, holistic practices, products, and services. Leadership is diverse and committed to providing space for affinity groups to host programs created by and for their communities. The cooperative also serves as an incubator space for small business development, including BIPOC and LGBTQIA+-owned businesses. As a cooperative, One Heart Wellness is owned and operated by the membership with a goal of ensuring membership fees are not a barrier to joining. More about One Heart Wellness.
Safe Spaces for BIPOC
Safe Spaces creates space for Black, Indigenous, and other People of Color (BIPOC) and Aspiring White Allies to connect, learn, and heal as we fight for our collective liberation. Safe Spaces strengthens individuals, communities, as well as institutions, businesses, and agencies through creating partnerships with other established racial justice organizations to provide guidance, resources, and physical and figurative space to work through systematic, systemic, and institutional prejudice and racism. Program offerings include: BIPOC Youth Programs (Read It & Eat it, Jol Indaba), Family Programs (Soul Food Programs, Game Nights), Adult Programs (BIPOC Women’s Group, Social Club), and special events from covering topics such as Mental Health in the BIPOC community during Winter months, BIPOC Women in Jazz and the Arts, and Growing Financial Literacy in the BIPOC Community. Learn more about Safe Spaces for BIPOC at: https://www.safespaces4.org/.
Storytelling Events for BIPOC and LGBTQIA2S+
Murphy Barney hosted virtual community storytelling and listening events designed for the Upper Valley to honor and share the healthcare-related experiences of BIPOC and LGBTQIA2S+ individuals. The events were in the style of town halls, but the storytellers were community members. Murphy generated the Health Equity Storytelling Report from the events that anonymously summarizes the experiences of storytellers and provides local healthcare providers and decision makers with a roadmap for improving services to BIPOC and LGBTQIA+ community members. By hosting community storytelling events, healthcare institutions receive clear guidance enabling them to provide compassionate, culturally informed, equitable health services. When healthcare institutions listen to the stories of their communities, policies begin to reflect the expressed needs of those they serve. More about Murphy Barney and the storytelling events.
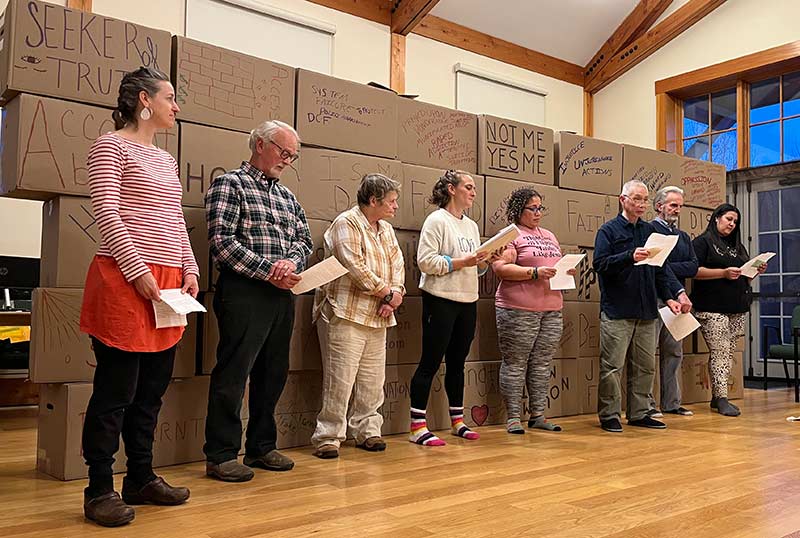
Telling My Story
Telling my story hosted three intensive workshops (14 hours over three days) with mental health providers and community members in the Upper Valley that addressed the urgent need for mental health providers to expand awareness and cultural competency with respect to BIPOC and LGBTQIA+ communities and individuals. Telling My Story workshops were aimed at increasing the cultural competencies, equity orientation, and overall accessibility of mental health providers towards marginalized people. “We do not expect to be able to educate providers on every element of the experience of being marginalized. Rather, we hope to instill awareness of privilege, power, the need to listen, and the need to act to build a more just society.” More about Telling My Story.
Unlikely Riders
Unlikely Riders brings folks together to break and reduce a sense of isolation, foster community connection and conversation, and improve mental wellbeing through investing and supporting BIPOC and LGBTQIA community members with no cost access to winter recreation, education and resources. The grant supported Upper Valley events like community ski and ride days allowing members to ski and ride at no cost, including community instruction and gear (winter layers and snow gear). Our intention through this programming is for folks to be in affinity to build joyful and fulfilling relationships with outdoor spaces and winter in Vermont, New Hampshire, and the Upper Valley. Our work is often in places (ski areas) that have historically been exclusive, inaccessible, and unwelcoming to Black, Indigenous, and People of Color, poor and working-class people, and queer and trans BIPOC folks. Our organization is rooted in creating long-term belonging, healing, and joy through relationship building with winter, snow recreation, and outdoor movement and our leadership is currently all LGBTQIA+ BIPOC folks, two of whom grew up in the Upper Valley area. Learn more about Unlikely Riders at: https://www.unlikelyriders.com/.
Windsor Central Supervisory Union (WCSU)

Student members of Woodstock Middle School/High School’s Queer Straight Alliance (QSA) designed and hosted a Queer Prom open to students at several nearby schools. The dance provided a safe, happy experience for students who might otherwise not attend such events and allowed them to make a typical high school experience uniquely their own. The event’s goals were to decrease isolation and loneliness and increase a sense of belonging, worth, and self-respect. Mental health and LGBT+ service providers also staffed booths and tables at the dance, helping to connect students to resources that can support their mental and physical health long past the event itself. By building relationships with other schools in the region, the hope is that this can become an annual event with shared responsibility for planning.
—-
The Public Health Council has been honored to participate in this work over the past few years. We hope the Upper Valley will rally around the people and organizations who have taken this opportunity to build programming to address the isolation and discrimination experienced by too many of our neighbors. By supporting this work, we make our communities stronger and healthier.