NH Opioid Addiction Prevention, E-Resources, and Support Website
 In the spring of 2017, a group of Dartmouth students participated in a Neuroscience class, “Motivation, Drugs, and Addiction.” They were intrigued by the social ramifications of their classroom learnings. To explore their interests, they compiled a lot of useful information. The students then decided to share that information by designing a website. That site, NH Opioid Addiction Prevention, E-Resources, and Support (NHopes), is a collaborative effort between students at Dartmouth College, local researchers, and New Hampshire community organizations. All these partners seek to provide accessible scientific information regarding the current opioid epidemic in NH. NHopes is designed to be a welcoming, informative experience for those interested to explore and learn about the extent of the opioid crisis, how opioids act on the body, and about recovery and resource options.
In the spring of 2017, a group of Dartmouth students participated in a Neuroscience class, “Motivation, Drugs, and Addiction.” They were intrigued by the social ramifications of their classroom learnings. To explore their interests, they compiled a lot of useful information. The students then decided to share that information by designing a website. That site, NH Opioid Addiction Prevention, E-Resources, and Support (NHopes), is a collaborative effort between students at Dartmouth College, local researchers, and New Hampshire community organizations. All these partners seek to provide accessible scientific information regarding the current opioid epidemic in NH. NHopes is designed to be a welcoming, informative experience for those interested to explore and learn about the extent of the opioid crisis, how opioids act on the body, and about recovery and resource options.
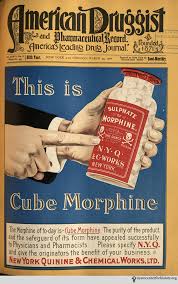
The website uses info-graphics and simple explanations to explain who is affected by the opioid epidemic, what is happening in the epidemic, and why opioid use has exploded.
Samples of NH Opioid Website Content
Hotspot Study
Dr. Lisa Marsch and colleagues at the Dartmouth Center for Technology and Behavioral Health conducted a study in NH designed to understand what gave rise to the opioid crisis. She and her team interviewed 75 Fentanyl and heroin users and 36 emergency personnel from the fire, police, and medical departments. See more…
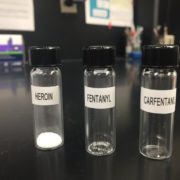
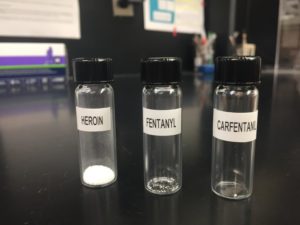
Carfentanil is an analog of fentanyl that is 100x as potent as fentanyl. Carfentanil has recently been reported in New Hampshire and has been attributed to 6 deaths so far in 2017. Carfentanil is lethal at small doses compared to both heroin and fentanyl (see image), and it is resistant to overdose reversal drugs.
A Social Impact Practicum
This site is made possible through the Social Impact Practicum (SIP) initiative at Dartmouth’s Center for Service. This program integrates community-driven opportunities for experiential learning into undergraduate courses at Dartmouth College. For more information, please contact Ashley Doolittle, Ph.D.
Partnering with Our Community
The Dartmouth students partnered with ALL Together to build this website. ALL Together is recognized as the Substance Misuse Prevention workgroup of the Public Health Council of the Upper Valley. It is also nationally recognized as a Drug Free Communities Coalition. ALL Together is supported by the New Hampshire Bureau of Drug and Alcohol Services, the New Hampshire Charitable Foundation, the Substance Abuse and Mental Health Services Administration (SAMHSA) and by Dartmouth-Hitchcock.