For the past 18 months, Emma Hartswick, one of the student interns profiled in this article, has worked with the Public Health Council as an Upper Valley Social Entrepreneurship Fellow from the Dartmouth Center for Service. She has been a real asset to our work and we look forward to having her back on staff after what sounds like a wonderful summer in Boston. — Alice Ely
Article Written By Charlotte Albright (Used with Permission)
Twelve students spent the summer in Boston on the front lines of public health. As participants in a 10-week program sponsored by Dartmouth Center for Service in partnership with Dartmouth Partners in Community Service, they interned in community health centers and other nonprofit organizations, serving the city’s most vulnerable populations—people living on the streets or in shelters, refugees, and low-income families.
“All of our internship programs seek to develop leaders capable of meeting social challenges in either the public or private sector,” says Tracy Dustin-Eichler, the assistant director for nonprofit careers at the Center for Service. “Boston is a hotbed for innovative solutions to pressing health care problems.”
Learning How to Help
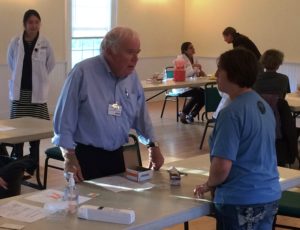
Intern Emma Hartswick ’17 began most workday mornings at a foot clinic run by Boston Health Care for the Homeless in St. Francis House, a daytime shelter that offers a wide range of social services. Interns and local nursing students do triage, caring for tired and damaged feet, which can flag more serious health problems that might otherwise go undiagnosed—especially in homeless people.
In a small, windowless room with a few chairs, soaking basins, and a supply cabinet, Hartswick greeted clients and posed a few basic questions—names, ages, health issues—before offering socks, anti-fungal foot powders, and soothing creams.
A middle-aged man limped in, sat down, took off his shoes, and soaked his feet in a basin as Hartswick rummaged in a drawer for white cotton socks. He said it was exhausting, walking the streets of Boston in all kinds of weather, using a cane.
“They help take care of my feet here,” he explained. “They take my blood pressure, too, and I appreciate the kind words they have to say.”
Hartswick also worked in two other community health clinics, doing intake assessments and providing child care for patients. A sociology and biology major, she’s thinking of attending medical school and is considering a master’s degree in public health.
“I am really interested in the social determinants of health, in the intersection of somebody’s life circumstances and their overall wellbeing,” Hartswick says. She often chats with homeless people as she walks through Boston Common to St. Francis House. “People assume they are unemployed, but a lot of them are working—they just can’t afford housing,” she says.
Connecting Students and Alumni
In addition to placing students in clinics, the Center for Service connects them with Dartmouth alumni working in medicine. Each intern is paired with an alumni mentor. Once a week, the 12 interns, who lived in dorms rented from Boston University, gathered for a dinner seminar, either to make presentations and share stories about the places where they are working, or to listen to a talk by a leader in health care or public policy.
“Local alumni are key co-educators with us in this program,” says Dustin-Eichler. A larger alumni group, called Dartmouth Partners in Community Service, provides funding and mentoring connections for this and other internship programs.
In a downtown office building one warm night, the interns met Joshua Greenberg ’86, vice president of government relations at Children’s Hospital, and Jay Gonzalez ’93, the CEO of CeltiCare Health Plan. Both men have been forceful advocates for broadening access to affordable health care in Boston. Gonzalez served as budget chief for Massachusetts during the governorship of Deval Patrick, chairing the board of Health Connector, which was a model for the Affordable Care Act. He traces twists and turns in his career path, advising interns to consider public service.
“If you have the chance to work in government,” he advised the students, “do it. And if you can prove you can take on any responsibility, you will get it, and then some. The opportunity to really have an impact on people in the public sector is unlike anywhere else.”
Seeing Policy in Practice
Some of the interns are more interested in health policy than in hands-on care. For example, at DotHouse Health, in Dorchester, Arvind Suresh ’19 and Yingna Wang ’17 updated patient and provider lists. They also worked on an app to help patients find social services.
The interns shadowed doctors, which, for Wang, was eye opening, especially regarding the impact electronic medical records are having on medical practice.
“I think it’s really important for policy people to understand what doctors do on a daily basis, and I will take that understanding with me as I pursue a career in public health,” Wang said.
Suresh gathered data about a device being used on a trial basis to determine an infant’s height. As each baby lay on a tabletop measuring board, Suresh watched a nurse use sliders to mark the head and feet. He was trying to learn whether this method is more accurate than the clinic’s current practice of using markers and paper to measure babies.
“I am learning so much about public health from different perspectives. We’re also seeing what are the most important issues that we can take on in the future,” Suresh says.
That future will present challenges as public health care workers try to meet the needs of an increasingly diverse population. About one-third of the clients at DotHouse are of Vietnamese descent. There are also many Spanish speakers.
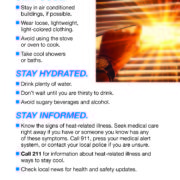
“Providers here are very aware of language and cultural barriers to health care,” said Wang. She and Suresh made sure that the practical tips about health and wellness they post on waiting room bulletin boards get translated into several languages.
For Suresh, managing that flow of multi-lingual information has deepened his understanding of the challenges patients in this clinic face—not just health problems, but other issues, like housing and employment, which affect their wellbeing.
“It’s extremely interesting to see how everyone here needs to think about all the things that other people need and prepare for that every day,” Suresh says.
The full list of summer community health interns:
- Yingna Wang ’17, DotHouse Health
- Aneeq Chaudhry ’19, Health Resources in Action
- Daniel Finch ’17, East Boston Neighborhood Health Center
- Emma Hartswick ’17
- Arvind Suresh ’19, DotHouse Health
- Wafaa Ahmed ’17, Codman Square Health Center
- Angela Liu ’17, Baraka Community Wellness
- Allessandra Ledoux ’17, Codman Square Health Center
- Noah Manning ’17, Health Leads
- Allyson Block ’19, East Boston Neighborhood Health Center
- Amrit Ahluwalia ’19, The Boston Living Center
- Margo Putnam ’19, The Women’s Lunch Place
Editor’s Note: Charlotte Albright is a writer in the Dartmouth College Office of Communications. This story was originally published on Dartmouth News, the college’s news website. The photograph is by Robert Gill, who also works in the Communications Office.
 Lebanon, NH — On October 19, 2016, the Mascoma Valley Health Initiative (MVHI) became part of the Public Health Council of the Upper Valley. “This change makes the organization stronger and will help us fulfill our mission of making Upper Valley communities better and healthier places to live,” said Alice Ely, who now becomes the Executive Director of the Public Health Council, served as the Executive Director of MVHI and the Coordinator of the Public Health Council for the past six years.
Lebanon, NH — On October 19, 2016, the Mascoma Valley Health Initiative (MVHI) became part of the Public Health Council of the Upper Valley. “This change makes the organization stronger and will help us fulfill our mission of making Upper Valley communities better and healthier places to live,” said Alice Ely, who now becomes the Executive Director of the Public Health Council, served as the Executive Director of MVHI and the Coordinator of the Public Health Council for the past six years.