APHA Annual Meeting: PHC Was There
This November, two Public Health Council of the Upper Valley members and several individuals from the Health Promotion Research Center at Dartmouth (HPRCD) presented local work at the American Public Health Association (APHA) Annual Meeting in Atlanta, Georgia. The event, which took place from November 4th – 8th, centered on the overarching theme: Climate Changes Health. Throughout the conference, keynote speakers explored how our changing climate impacts human health both directly and indirectly, and how it creates and perpetuates health disparities across our country and the world. The APHA Meeting also includes sessions that cover many other public health topics. With nearly 12,000 people in attendance, the APHA Meeting allowed attendees to network with, learn from, and educate one another.
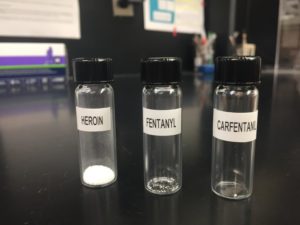
Tobacco and Electronic Nicotine Delivery Systems Use
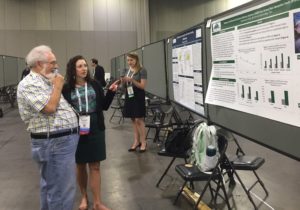
Stephanie Kelly discussing ENDS use in NH youth with Dr. Stan Glantz, professor, tobacco researcher, and activist based at University of California, San Francisco.
Stephanie Kelly, of the HPRCD and PHC’s Oral Health Work Group, attended sessions on oral health and tobacco cessation efforts. Her poster presentation, titled “Tobacco and Electronic Nicotine Delivery Systems (ENDS) Use Among New Hampshire Youth, 2010-2015” discussed how New Hampshire youth’s patterns of e-cigarette use relate to national trends, and how prevalence of e-cigarette use varies by gender and high school grade level. Kelly’s poster was well received by other tobacco researchers, who drew connections between New Hampshire’s data and their own anecdotal experiences. [Stephanie’s Abstract]
APHA Members Learn About Rural Aging in Community Groups
Emma Hartswick, a former fellow at the PHC, also attended the conference to share a community listening project she conducted with Upper Valley residents. Her oral presentation, titled “Exploring Successes, Challenges and Next Steps for Rural Aging in Community Groups” featured the voices of local leaders who are working hard to help their neighbors retain their agency and autonomy as they age, despite the added challenges imposed by a rural environment.
When Hartswick began the project in the winter of 2015, her goals were to understand what services Aging in Community groups offered, how they provided them, and what the Public Health Council could do to support their important work. Looking back two years later, our community’s efforts to support older adults impressed people who attended the talk, and many supported our conclusion that large public health and clinical partners should turn to local organizations to set priorities and guide future work.
APHA Provides Exciting New Information
Now working as a Case Manager and Child Development Coordinator for Boston Health Care for the Homeless Program, Hartswick also attended sessions on mental health, substance use, social justice and maternal child health. “There was so much to learn! I’m really excited about the ideas and approaches I can take back to my team now.” Hartswick said she was struck by how interdisciplinary the conference was, with topic sessions often melding key themes from multiple areas.
Jam packed with posters, talks, booths, round tables and panels, the APHA Annual Meeting both sparked new questions and affirmed current ideas. “It was cool to see how many of our PHC priority areas were big topics of the Annual Meeting,” said Hartswick; “it made it feel like we’re heading in the right direction, on the cutting edge, but not alone.”