Exploring Community Health Priorities in the Upper Valley
 Improving community health is at the core of the mission of the Public Health Council of the Upper Valley. Most of our partners share this goal, but contribute in different ways to reaching that goal. Some partners are health care providers, some provide treatment for substance use disorders or mental illnesses, others support people in our communities who struggle with various social determinants of health.
Improving community health is at the core of the mission of the Public Health Council of the Upper Valley. Most of our partners share this goal, but contribute in different ways to reaching that goal. Some partners are health care providers, some provide treatment for substance use disorders or mental illnesses, others support people in our communities who struggle with various social determinants of health.
Every three years, the Public Health Council works with our many partners to update a set of regional priorities that answers the questions: What are the health issues our community members are most concerned about? How can we make a difference, especially by using the strength of our collaboration? And every three years, nonprofit hospitals, like Dartmouth-Hitchcock and Alice Peck Day Memorial Hospital, are required to complete a community health needs assessment and a community health improvement plan. Over the course of 2018, the Public Health Council was able to work with these hospitals, and others in our region, to complete a joint community health needs assessment. As we move into 2019, we continue to work together to explore more deeply what the assessment results tell us and how we can share in the work of making a difference.
The Greater Upper Valley Works Together
All nonprofit hospitals in American must complete community health needs assessments and community health improvement plans. These plans identify priority needs in hospital service areas and direct the hospital’s community benefit investment in their communities. However, our region has taken this work to a new level, by combining the resources of six health care institutions in the region to complete a large scale assessment. These institutions include Dartmouth-Hitchcock, Alice Peck Day Memorial Hospital, Visiting Nurse and Hospice for VT, Mt. Ascutney Hospital and Health Center, Valley Regional Healthcare, New London Hospital. The purpose is to identify community health concerns, priorities and opportunities for community health and health care delivery systems improvement. By gathering the same data across a large region, we are able to see similarities across our many communities, identify differences (or disparities), and coordinate strategies to address concerns.
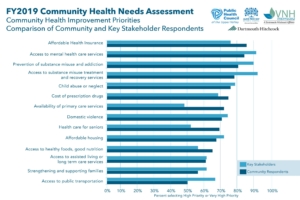
Upper Valley Community Health Needs Assessment
The Upper Valley Community Health Needs Assessment generated for the Dartmouth-Hitchcock and Alice Peck Day primary hospital service areas covers 19 municipalities in Vermont and New Hampshire, with a total resident population of 69,467 people. Data came from surveys of community residents; a direct email survey of key stakeholders and community leaders; a set of community discussion groups; a behavioral health needs assessment conducted in 2016; and a review of available demographics and health status indicators. The New Hampshire Community Health Institute conducted the survey, data analysis, and report generation. Throughout the process, they were careful to focus on vulnerable and disproportionately served populations in the region. We wanted to ensure all populations that could experience limited access to health-related services or resources due to income, age, disability, and social or physical isolation were seen in the results.
Taking It Back to the Community
Beginning in January 2019, the Public Health Council has been working with partners at Dartmouth-Hitchcock, Alice Peck Day Memorial Hospital, Visiting Nurse and Hospice for VT to share the results with members of our communities and get input into where we go from here. In January, we co-hosted two Community Health Improvement Summits open to all community residents to review the priorities emerging from the recent results and share thoughts about what the results tell us, what opportunities we have to address them, and what strategies we might help. In February, we took advantage of a training co-sponsored with the Special Needs Alliance, Cultural Competence with Disabilities, to address the priorities from the perspective of people living in our communities with disabilities.
Capturing Input from Our Communities
Notes from all the discussions held so far are available for review. You will find links to these notes below.
Community Summit Notes from January 18 @ 5:30 pm (Dwinell Room) and Public Health Council Partner Meeting (open to public), January 18 @ 9:00 am (Tracy Hall)
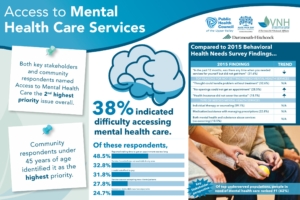
Mental Health Services
Substance Misuse
Child Abuse and Neglect
Primary Care Services
Domestic Violence
Health Care for Seniors

Discussing issues of child abuse and neglect with Nancy Bloomfield, of The Family Place, as a subject matter expert.
Forum at Cultural Competency with Disabilities Training, February 8 (Kilton Library)
Mental Health
Domestic Violence/Child Abuse and Neglect
Primary Care Services
Over the next several months, we will continue to present results to community groups, looking for insights into what work the results tell us to do. Each of the organizations collaborating on this work will develop their own Community Health Improvement Plan. Most of these plans will be completed by the end of 2019 or soon thereafter.
For more information about the community health improvement planning process or ways you can participate, please contact Alice Ely at the Public Health Council.