Transforming Behavioral Health Care Across New Hampshire
On January 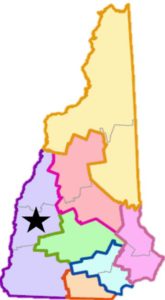 25th, about 75 individuals came together from across Region 1 to kick-off the next five months of work to begin transforming behavioral health care for our Medicaid enrolled residents. Through hands-on, small group exercises, teams worked together to discuss opportunities, challenges and goals of our region as we partner in driving integration, improving coordination and expanding capacity. Shared themes emerged across all project team groups including an emphasis on patient-centered care, increased access, improved communication among providers and with patients, enhanced and embedded wraparound services especially housing and transportation, innovative technology solutions, care management roles, peer recovery coaches, and a progressive, proactive and positive culture. Thank you to everyone for their active engagement in this kick-off!
25th, about 75 individuals came together from across Region 1 to kick-off the next five months of work to begin transforming behavioral health care for our Medicaid enrolled residents. Through hands-on, small group exercises, teams worked together to discuss opportunities, challenges and goals of our region as we partner in driving integration, improving coordination and expanding capacity. Shared themes emerged across all project team groups including an emphasis on patient-centered care, increased access, improved communication among providers and with patients, enhanced and embedded wraparound services especially housing and transportation, innovative technology solutions, care management roles, peer recovery coaches, and a progressive, proactive and positive culture. Thank you to everyone for their active engagement in this kick-off!
Our work in Region 1 is part of a statewide effort to address costly concerns about how our behavioral health and health care systems respond to our most vulnerable people. Widespread variability currently exists in the availability and accessibility of both general and behavioral health services, including those for substance use disorders, across the state of New Hampshire and especially for the Medicaid population. Poor coordination among providers further inhibits availability of these needed services and treatments – even in those communities with sufficient resources. As a result, patients and families struggle to schedule and keep convenient appointments; navigate among providers, offices and agencies; facilitate or ask for communication between providers; or receive all of the care they need in a timely manner.
Providers are often as frustrated as the patients and families; they find that the system makes it increasingly challenging for them to provide patient-centered care and fulfill their missions as care providers.
The State of New Hampshire, responding to a call to action, was awarded federal dollars (the Delivery System Reform Incentive Payment Medicaid 1115 Waiver – also known as the DSRIP Waiver) to improve behavioral health services across the state of New Hampshire for those insured by Medicaid. The state has created seven regions through which these funds will be invested over the next four years, with some of the funds awarded only if care is improved.
Transforming Behavioral Health Care in Region 1
Region 1 consists of Sullivan County, the Greater Monadnock region, and the Upper Valley. The State intends these funds be used to redesign the delivery of care through the integration of behavioral and general health services, with a specific emphasis on helping patients with substance use disorders and serious mental illness. Almost 50 agencies, including advocacy groups, public health advisory councils, housing agencies, municipal offices, clinical providers, substance use disorder centers and mental health workers, have united to create innovative solutions to address the systemic problems (both statewide and locally) that lead to poor health outcomes. We hope the changes we make will, in turn, benefit the whole community, improving health for everyone and not just the Medicaid recipients.
The work is divided into several broad categories:
- Integration of mental health and substance use treatments into primary care practices to provide one-stop care and comprehensive care plans – making it easier to coordinate among clinicians and service providers
- Development of a simple, confidential information system that allows for efficient flow of information among providers
- Expansion of intensive substance use disorder treatments and services – availability and access
- Improvement of care during transitions from hospital to community – ensuring patients do not “fall through the cracks” upon discharge
- Education and training of a new group of mental health workers to help coordinate and manage care
- Improvement of the care system for people with complex mental and physical disabilities
- Creation of an alternative payment model to ensure coverage for all integrated services
Our communities currently face a health crisis; this grant provides the necessary support to find solutions. Working together, as partners, we will meet this challenge by creating innovative paths to ensure all patients receive the right care at the right time in the right place. Together, we are transforming behavioral health care for all.
For more information about this initiative, see this article posted on the DHMC website in November 2016.
To contact initiative staff, you can reach out to Ann H. N. Landry, Executive Director, or Jessica Powell, Project Manager.


Leave a Reply
Want to join the discussion?Feel free to contribute!